Iridodonesis is a slight, visible trembling of the colored part of your eye, the iris, that usually means the lens inside the eye is not as stable as it should be. In many people, it is not dangerous by itself; however, it is a sign that your eye needs a careful examination to ensure the lens and other structures are healthy. With the correct diagnosis and monitoring or treatment, most patients can preserve their vision and maintain comfort.
This guide explains what iridodonesis is, how it can affect your vision, and the main treatment options your ophthalmologist may recommend.
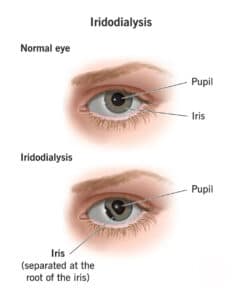
Iridodonesis means the iris trembles or “wobbles” when the eye moves. Instead of staying smooth and steady, the iris ripples slightly with each eye movement.
This iris tremor happens when the natural lens, or an artificial lens implant after cataract surgery, is not firmly supported. The lens may be partly out of position, or the tiny fibers that normally hold it in place may be weak or damaged.
On its own, this movement is often subtle. Many people do not notice it in daily life. It is commonly first seen by the eye doctor during a slit lamp exam.
How Iridodonesis Affects Vision

-
Glare and halos, especially around lights at night
-
Shimmering or “jiggling” vision
-
Light sensitivity
-
Intermittent blur
-
Monocular double vision, where you see a double image in one eye
-
Eye strain or fatigue, especially after reading or driving
When the lens is unstable, it may not sit in its intended position. The iris has less support behind it, so it moves more with each eye motion. A lens that is off-center can alter the way light focuses on the retina, potentially causing ghosting, blur, or changes in prescription.
Common Causes of Lens Instability
Several conditions can lead to lens movement that shows up as iridodonesis:
-
Prior eye trauma or blunt injury
-
Advanced cataracts or changes in the lens capsule
-
Weak lens support fibers, sometimes from conditions such as pseudoexfoliation
-
High myopia (very nearsighted eyes), which can stretch the eye structures
-
Lens implant (IOL) that has shifted, tilted, or become partially dislocated after cataract surgery
-
Less commonly, inherited connective tissue disorders such as Marfan syndrome or Weill-Marchesani can weaken the fibers that hold the lens in place.
Your ophthalmologist will examine you for these possible causes during a comprehensive eye exam.
When to Call Your Eye Doctor
You should contact your eye doctor promptly if you notice:
-
Sudden blurred vision after a hit or injury to the eye
-
A dark crescent or shadow at the edge of your pupil
-
A dramatic increase in glare, halos, or double vision
-
A new curtain, shadow, or missing area in your field of vision
These changes can be signs of significant lens displacement or a retinal problem. They need fast evaluation so your doctor can protect your sight.
How Iridodonesis Is Diagnosed

-
Your visual symptoms
-
Any history of eye trauma
-
Any prior eye surgeries, especially cataract surgery
A typical workup may include:
-
Slit lamp exam to watch the iris and lens position closely as the eye moves
-
Refraction and pupil tests to see how your focus, clarity, and pupil reactions are affected
-
Corneal topography or anterior segment imaging, if needed, to map the shape of the front of the eye and the position of the lens.
-
Retinal exam to rule out back-of-the-eye causes of blur, flashes, or shadows
These tests help your surgeon determine whether careful monitoring is sufficient or if active treatment is necessary.
Treatment Options for Iridodonesis
The main goals of treatment are to stabilize the lens or lens implant, protect the eye, and improve the quality of your vision. Your plan depends on:
-
How stable the lens or IOL is
-
How much is your vision affected
-
How bothersome your symptoms are
Your ophthalmologist will tailor the recommendations to your specific eye needs and daily requirements.
Conservative Management
If the lens is still well centered and your vision is good, your doctor may suggest a conservative approach. This can include:
-
Lubricating eye drops to improve comfort and reduce surface dryness
-
Tinted or polarized glasses to cut down glare and halos
-
Regular, scheduled exams to monitor lens position and eye health
In these cases, iridodonesis is more of a “warning sign” that the lens support is weaker, rather than an emergency in itself. The focus is on comfort, protection, and monitoring changes over time.
Surgical Repair and Lens Stabilization

Depending on the situation, your surgeon may:
-
Reposition the IOL and secure it with sutures or by attaching the lens to the iris or sclera (the white of the eye)
-
Exchange the IOL for a different design that better supports weak lens structures
-
Use capsular devices, such as capsular tension rings, to strengthen the natural capsule that holds the lens
At the same time, your doctor may address corneal dryness or other surface issues that exacerbate glare. In every case, the goal is to choose the least invasive option that can restore lens stability and improve visual quality.
Iridodonesis After Cataract Surgery
After cataract surgery, an iris tremor can be a sign that the lens implant has shifted or that the capsule and support fibers are not strong enough. Mild cases, where the lens is still centered and vision is clear, can often be watched with regular exams.
If the lens implant is decentered or dislocated, your surgeon may recommend:
-
Scleral fixation (gently attaching the IOL to the sclera)
-
Iris fixation (attaching the IOL to the iris in a controlled way)
-
IOL exchange, sometimes using newer techniques that secure the lens within the eye wall
These procedures aim to recenter or replace the implant, reduce lens movement, and calm the iris. The goal is a stable optical system, fewer glare and blur symptoms, and a comfortable eye.
For more technical information, especially for eye care professionals, the American Academy of Ophthalmology has a detailed review of traumatic lens dislocation and lens instability.
Recovery and Long-Term Outlook

-
Lubricating drops
-
UV-blocking sunglasses
-
Regular comprehensive eye exams to track lens position
After surgical stabilization, many patients notice an improvement in focus and reduced glare as healing progresses. Recovery time depends on the specific procedure, the health of your eye, and whether other conditions, such as glaucoma or retinal disease, are present.
Long-term follow-up is essential. Your doctor will:
-
Check lens stability
-
Monitor eye pressure
-
Look for any new changes in the cornea or retina
With proper care, many people can maintain good vision and do very well.
FAQ About Iridodonesis
Is iridodonesis dangerous by itself?
Not usually. Iridodonesis is a sign that the lens support has changed. Your doctor will examine the eye to decide whether the natural lens or lens implant needs closer monitoring or stabilization.
Can eye drops fix it?
Drops can improve comfort, reduce dryness, and alleviate glare, but they do not address the underlying lens instability. Surgical stabilization is considered when vision, lens position, or both are clearly affected.
Will it go away on its own?
If the support structures are weak or damaged, the iris tremor usually persists. When the lens or IOL is stabilized surgically, the movement often becomes much less noticeable or clinically unimportant.
Is this the same as a cataract?
No. A cataract is a clouding of the natural lens. Iridodonesis is a movement of the iris that often indicates changes in lens support, including after cataract surgery if a lens implant is off-center.
How is iridodonesis diagnosed?
Your ophthalmologist diagnoses it during an eye exam by watching how the iris moves when you look in different directions. They may also use special imaging and a dilated exam to check lens position and look for related problems such as lens subluxation or retinal issues.
How soon can I return to normal activities after surgery?
Most patients can resume many normal activities within a few days, although exact timing depends on the procedure and your overall eye health. Your surgeon will provide you with specific instructions regarding driving, heavy lifting, exercise, and eye protection to ensure a safe recovery.
Next Steps for Your Eye Health
If you notice shimmering vision, new glare, or have been told you have iridodonesis, it is essential to schedule a comprehensive eye exam. Your ophthalmologist can confirm the cause, explain whether simple monitoring, glare control, or surgical stabilization is best, and build a plan that matches your vision needs and long-term goals.

